Did you know, that one-month post-COVID-19 outbreak and 2/3 of Australians reported being anxious and stressed while 50% reported being depressed.
These are incredible stats, and these stats are being reflected in our clinic, with the vast majority of our patients reporting feeling anxious, stressed and depressed.
With stress, anxiety and depression symptoms on the rise in Australia, the ability to regain optimal health through health-promoting habits, such as eating a good diet, sleeping well, exercise and movement, and oral therapeutics, are not enough. increasingly we’re seeing the need for complementary care, such as therapy and mindfulness programs.
These conditions (anxiety, stress, depression) are associated with several comorbidities, such as cardiometabolic conditions, gastrointestinal disorders, and pain conditions, to name a few.
| Physical | Psychological | Behavioural |
| Changes in weight | Crying spells | Anhedonia |
| Changes in appetite/cravings | Constant worrying | Withdrawal from family and friends |
| Sleep disturbances | Mood swings | Relying on substances e.g., alcohol, drugs – stimulants/sedatives |
| Fatigue | Irritability | Psychomotor agitation e.g., constant pacing, tapping |
| Shortness of breath/rapid breathing | Lack of concentration | |
| Chest/body pain | Indecisiveness | |
| Low sex drive | Feeling overwhelmed | |
| Gastrointestinal symptoms |
Both conditions have the same core neurobiological underpinning – namely, microgliosis.
Microgliosis is when the microglia immune cells in the brain are converted into a pro-inflammatory state, which over time can lead to changes in brain architecture. Many people are aware of the role of serotonin, due to the rising popularity over the last 20 years of SSRIs (selective serotonin reuptake inhibitors). The narrative went like this: What causes depression? Brain malfunction caused by serotonin deficiency. How do you repair your brain chemistry? Drugs, namely SSRIs. It was a narrative that took hold, and undoubtedly helped many people escape, at least momentarily, from the throes of depression and anxiety. However, what we know now is that over time, the effectiveness of these drugs wanes. The band-aid has to be ripped off eventually, and the underlying causes need to be addressed.
Serotonin is not the only neurotransmitter that’s disrupted, glutamate and GABA are also key players. For example, lower levels of GABA in the brain give us that feeling of indifference and lack of joy – we can’t seem to derive pleasure from anything because there’s always this underlying fear. Sound familiar? This is often followed by sleep disturbances, which further exacerbates symptoms, leaving us to wonder where to turn next.
We see this all the time in the clinic when we put our patients through in-house testing (which we offer patients free of charge). We can see the areas of the brain that are typically affected – the pre-frontal cortex almost always has lower volume (due to atrophy) and the limbic system is overactivated (i.e. the amygdala), and this is a great indicator of anxiety and depression.
So what’s the answer?
Thankfully we have oral therapeutics that we can utilize, and certain herbs, such as passionflower, magnolia, and lemon balm have been shown to have measurable effects on lowering psychological symptoms of anxiety, and we do see great results using herbs with our patients.
However, as practitioners, we want to get to the core of what’s really going on – what the key drivers are. Often this means addressing HPA axis dysfunction and inflammation.
Most of you will be familiar with the negative effects of chronic inflammation but let me just give you a little primer in HPA axis activation, so you are aware of what I’m talking about.
All sensory information is processed in the brain, no surprise there. This includes stress, or perceived stress, as well as perceived threats. This information is processed in the ancient part of our brain called the limbic system. One of the key organs of the limbic system is the amygdala. The amygdala processes the sensory information and sends a stimulatory message to the hypothalamus (the H in HPA axis). Glucocorticoids (stress hormones) are then pumped out to deal with the stress response. Over time, chronically elevated levels of glucocorticoids result in a downregulation of glucocorticoid receptors, and you end up with continual elevation of glucocorticoids – i.e chronic stress. This disrupts the serotonergic system, meaning less serotonin is available or taken up in the brain. Glucocorticoids also get into the amygdala and increase glutamate, resulting in anxiety and depression. Unfortunately, we also lose a lot of minerals as a consequence of elevated glucocorticoids, especially magnesium.
Since magnesium helps increase GABA and protects us against the effects of excess glutamate, having insufficient levels of magnesium will further drive the imbalance between glutamate and GABA.
So what are we doing about it?
As I said at the top, cleaning up the diet and using specific herbs is often very useful, but as you can appreciate, addressing underlying stress is going to be the deciding factor in getting to the root cause of the mood disorders.
That’s why we’re increasingly recommending meditation to our patients. We have started rolling out Vedic Meditation courses at NatMed, under the guidance and expertise of Vedic Meditation teacher Dr. Lana Loxton. Vedic meditation has been shown to have profound effects on the stress response at a dose of just 20 mins twice a day. If you are interested in discovering more about Vedic meditation, Dr. Loxton, follow NatMed on Facebook or Instagram to learn when the next Introduction to Meditation course is.
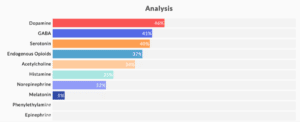
Additionally, we have started tailoring specific amino acid therapy to patients presenting with mood disorders. This is being done using a Mood Disorder Appraisal questionnaire consisting of 66 questions. These are carefully calibrated questions, the answers to which provide clues as to deficiencies in certain amino acids and thus neurotransmitters an individual might have. A sample report might look something like this:
In this case, we can see that dopamine, GABA and serotonin deficiencies are most prominent. We can then use these results to compound a bespoke amino acid powder containing specific amounts and ratios of amino acids to correct for these deficiencies.
If you are suffering from anxiety, depression, stress, anger, agitation, please get in touch with the clinic and we’ll be happy to send you the questionnaire and put together a bespoke compound to address your specific neurotransmitter deficiencies.
Click the ‘Book Now’ button below to book a 15-minute scoping session.